Cervical cancer screening can now include “self-swab” HPV tests, according to updated guidelines published Thursday by the American Cancer Society.
The change, experts hope, will encourage more women to undergo regular screening for the cancer by giving them an alternative to a speculum exam.
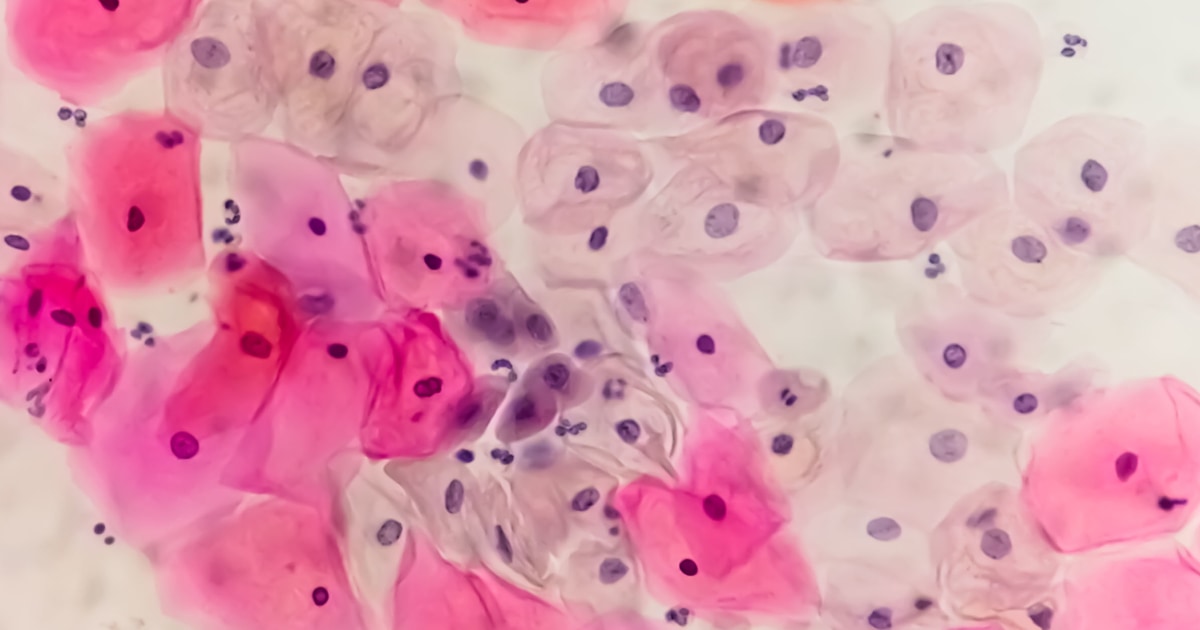
Testing for HPV, or human papillomavirus, has supplanted the Pap test as the preferred method for cervical cancer screening. Pap tests (also called cytology) involve collecting cells from a patient’s cervix during a pelvic exam, a process some women find uncomfortable and even painful.
“HPV is such a strong indicator of cervical cancer, we know now that screening for HPV is screening for cervical cancer. This gives more options to women,” said Jane Montealegre, an associate professor of behavioral science at the The University of Texas MD Anderson Cancer Center in Houston, who was not involved in the updated guidelines.
HPV testing has typically used a similar approach to a Pap test, using cells collected from the cervix. Since 2024, however, the Food and Drug Administration has approved three self-administered HPV tests, including one that can be done at home.
Cervical cancer rates have been steadily falling in the United States since the 1970s, largely because of improved screening and widespread use of the HPV vaccine since its approval in 2006. There are 40 different types of HPV that can infect the genitals, 13 of which cause nearly all cervical cancers. HPV testing focuses on the high-risk strains.
Despite falling rates of cervical cancer, more than 20% of American women aren’t up to date on screening, a JAMA Network Open study found. The self-administered tests allow patients to collect their own sample using a vaginal swab in a doctor’s office. One of the FDA-approved tests allows women to use the swab at home and mail it to a lab for analysis.
The self-administered tests allow patients to collect their own sample using a vaginal swab in a doctor’s office. One of the FDA-approved tests allows women to use the swab at home and mail it to a lab for analysis.
“A woman would be given a kit and could go some place, either the exam room or bathroom, and collect her own sample,” said Robert Smith, a cancer epidemiologist and senior vice president of early cancer detection science for the American Cancer Society. Smith was the senior author of the update.
Both the American Cancer Society and the U.S. Preventive Services Task Force — a group of independent doctors, nurses and public health experts who regularly review the latest scientific research and issue recommendations for everything from diabetes to cancer screening — recommend women screen for cervical cancer using HPV testing every 5 years. If the test is positive, a doctor will follow up with additional testing.
Both groups also say patients can be screened using a Pap test and a speculum exam every 3 years, or through using both methods every 5 years.
Where the two groups differ is when screening should begin: The American Cancer Society recommends women start this screening regimen at age 25, and not screen before that. The task force, whose recommendations influence what screenings insurance will cover, recommends starting the HPV screening schedule at age 30, and screening with cytology alone every 3 years between ages 21 and 29.
Montealegre said she does not expect the task force to change its stance on this, however, it is expected to update its guidelines for HPV screening to include self-administered tests.
Cervical cancer screening is covered under the Affordable Care Act, and Montealegre said the self-administered tests, at least those administered at a health clinic, will likely be covered by insurance.
“Primary HPV testing is already recommended by the USPSTF, so it is already covered by insurance, and they don’t specify how it has to be collected,” she said.
Both organizations recommending the HPV test as the primary way to screen for cervical cancer “indicates that there is growing agreement that it is the gold standard,” Smith said.
“We have known for years that primary HPV testing is much more efficient, now we are doing self-sampling to allow for better access,” said Dr. Diane Harper, a professor of obstetrics and gynecology and family medicine at the University of Michigan.
The American Cancer Society update also included clarification on when a woman can stop cervical cancer screening. Previously, both the group and the task force recommended screening up to age 65. The updated guidelines clarify that this should be the case only if a woman has had consistent screening, with negative results, for at least a decade.
“Despite clear recommendations on the importance of women being up to date with screening up to 65, very few women are,” Smith said. “It’s important for women to understand that there is a record they will want to have by the time they are 65 that will basically tell them it’s safe to stop screening for cervical cancer.”
Harper, who wasn’t involved in drafting the new guidelines, expects that in the coming years, cervical cancer screening will likely be done at even longer intervals.
“We have data showing now that in a highly vaccinated population, you can screen every 10 years, but we in the U.S. are lagging behind,” she said.